Situs Judi Slot Online Gacor Terbaru dan Terpercaya Mudah Menang 5 Lucky Lions
Situs Judi Slot Yang Gacor Terbaru 2023 Paling Gampang Menang 5 Lucky Lions
Five Lucky Lions ialah Situs Slot Gacor Terbaru dan Terpercaya 2023 Mudah Menang Jackpot Terbesar 2023 dari Habanero. Mesin slot gacor terpercaya yg di rancang sang Habanero. Game Slot penghasil Uang yang mempunyai 6 gulungan serta 4 baris. Ini adalah permainan varian rendah dan memiliki total 88 paylines. Fitur termasuk: putaran bebas dan pergantian liar.
Secara total slot jackpot terbesar ini memiliki 6 x4 serta 88 garis pembayaran permanen. Bo Slot Gacor Gampang Menang yang berwarna keemasan dan mengapung pada depan bangunan Cina bergaya kekaisaran yang tampak tradisional. Simbol pencar adalah drum merah, serta itu bernilai x100 yang cukup luar biasa berasal taruhan aslinya. Menjadikannya simbol permainan slot jackpot terbesar ini menggunakan nilai tertinggi.
Info Bocoran Rtp Slot Online Tertinggi Hari Ini Habanero 2023 5 Lucky Lions

Singa itu sendiri membentuk beberapa simbol bayaran tinggi asal permainan game slot bet kecil. Mainkan Link Slot Gacor Hari Ini Terpercaya Lucky Lions para member setia dapat meraih hingga 18 putaran gratis. Menggunakan 88 paylines buat dimenangkan, game demo slot ini menyenangkan buat berputar dari awal hingga akhir.
5 Lucky Lions dimainkan pada susunan 6 gulungan game online slot masing-masing dengan tinggi empat simbol. Karena delapan adalah angka keberuntungan pada takhayul Tiongkok, terdapat 88 garis kemenangan buat dimainkan. Pengembalian ke pemain rtp slot hari ini artinya sebesar 97,93%, yang dengan nyaman berada pada atas tolok ukur yg kami gunakan sebesar 96%. Volatilitas permainan ini sedang, yg berada pada ujung terendah dari apa yg mampu kami sesuaikan dengan strategi pilihan kami.
- Provider Slot Online: Habanero
- Nama Slot Gacor: 5 Lucky Lions
- Live Rtp Slot Terpercaya: 96.64%
- Volatility: sedang (3 dari 5 bintang)
- Paylines: 88 cara pembayaran
- Jackpot Maxwin: 4400x total taruhan
Fitur Game Slot Gacor Hari Ini Penghasil Uang Terbesar 2023 5 Lucky Lions
Five Lucky Lions ialah slot gacor hari ini yang indah. Menyenangkan secara visual dan di animasikan menggunakan baik dan menyenangkan buat dimainkan. Ini pula mempunyai pengembalian Rtp Slot Tertinggi yg sangat indah ke pemain sebanyak 97,93% serta volatilitasnya tidak mengerikan.
-
Fitur Simbol Wild Game Slot Terbaik
Pertama Simbol Wild game slot online dengan karakter anak laki laki yang sedang memainlan krenceng, akan menggantikan simbol apa pun kecuali Scatter.
-
Fitur Simbol Scatter Game Slot Paling Gacor
Kedua Meraih 3 atau lebih simbol slot terbaik di mana saja pada keliru satu gulungan. Ini pula akan memicu insentif putaran perdeo.
-
Fitur Free Spin Game Judi Slot yang Sering Menang
Ketiga Sebuah permainan hanya sebagus penawaran putaran gratisnya dan itu memang berlaku buat lima Singa Keberuntungan. Fitur spesifik ini terpicu waktu pemain mendarat di 3 atau lebih simbol pencar, yaitu gendang merah. Pemain game judi slot akan di arahkan buat memilih singa berasal 5 yg di tawarkan serta - tergantung pada pilihan mereka - akan memberi hadiah 8, 10, 12, 15 atau bahkan 18 putaran gratis.
 Situs Judi Slot Online Gacor Terbaru dan Terpercaya Mudah Menang 5 Lucky Lions
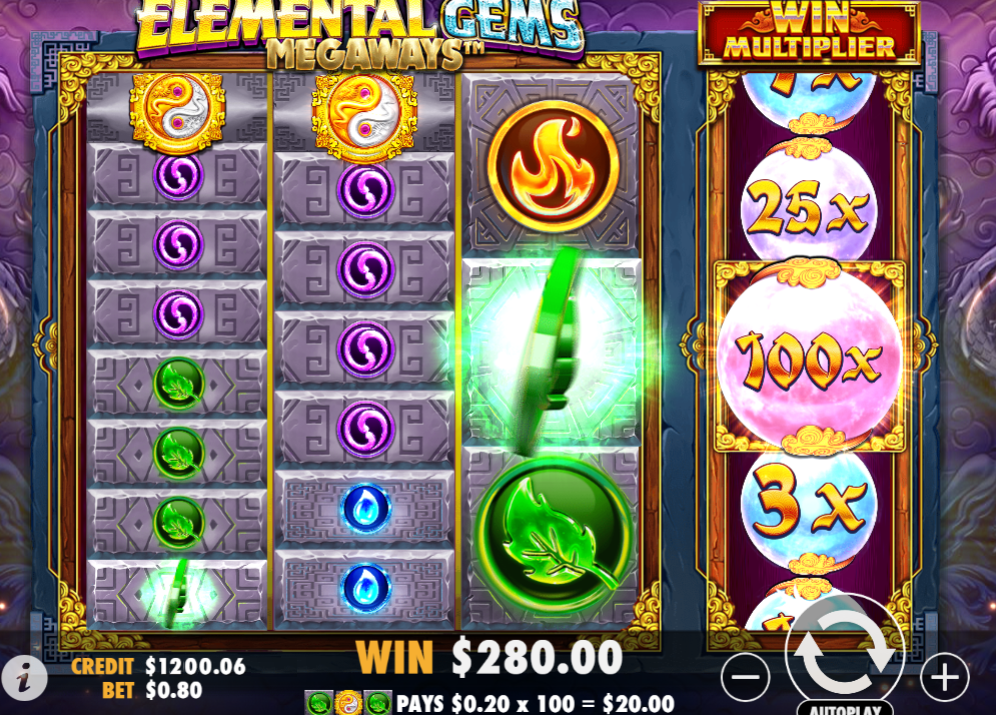
Situs Judi Slot Online Gacor Terbaru dan Terpercaya Mudah Menang 5 Lucky Lions  Situs Link Slot Gacor Maxwin Hari Ini Terpercaya 2023 Elemental Gems Megaways
Situs Link Slot Gacor Maxwin Hari Ini Terpercaya 2023 Elemental Gems Megaways  Situs Judi Slot Terbaik dan Terpercaya No 1 2023 Sugar Rush
Situs Judi Slot Terbaik dan Terpercaya No 1 2023 Sugar Rush  Situs Judi Slot Online Terpercaya 2023 Deposit Pulsa Tanpa Potongan Oriental Prosperity
Situs Judi Slot Online Terpercaya 2023 Deposit Pulsa Tanpa Potongan Oriental Prosperity  Situs Slot Gacor Maxwin Hari Ini Terpercaya 2023 Paling Banyak Menang Supermarket Spree
Situs Slot Gacor Maxwin Hari Ini Terpercaya 2023 Paling Banyak Menang Supermarket Spree